PREPARE programme
Our PREPARE programme will help you get ready for your oesophago-gastric surgery.
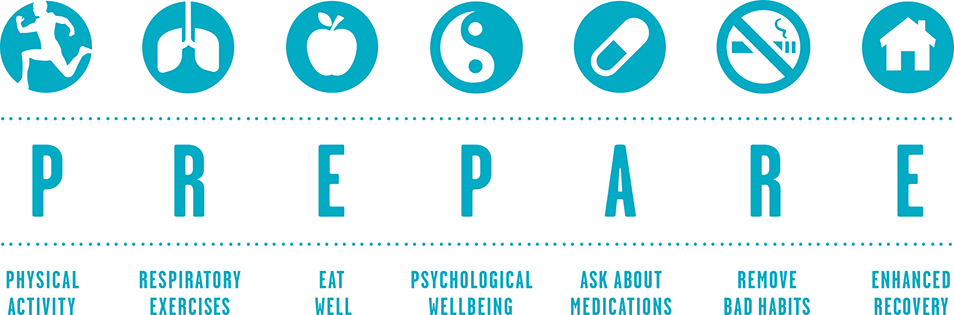
If you are having major cancer surgery, we may recommend that you take part in our PREPARE for surgery programme. The program will provide coaching and tailored support in the areas of:
- physical fitness
- respiratory exercises
- eating well
- psychological wellbeing
- your medication
- smoking and alcohol
- enhanced recovery after your treatment
Evidence suggests that preparing patients in these key areas improves outcomes and also enhances recovery. Poor physical performance and nutrition can increase the risk of complications after surgery and prolong recovery. Watch our video to learn more about the programme.
What will happen during the programme?
We will assess your medical, physical, psycho-social and nutritional wellbeing before you have surgery. Based on the results of your assessment, we create a personalised programme for you to work through.
Physical fitness
Evidence suggests that patients who maintain routine physical exercise before surgery have a reduced chance of complications and are more likely to have a quicker recovery.
During your first session your fitness will be assessed by an exercise specialist. This will involve a few simple assessments. We recommend that you wear loose clothing and trainers for this session as you’ll be asked to move around.
A personalised exercise programme will then be agreed based on the results of the tests. Your exercise programme will be home-based and monitored on a weekly basis through the return of your exercise adherence diaries and telephone contact from the exercise specialist.
Your exercise programme aims to increase aerobic capacity, muscle and core strength.
Respiratory exercises
Respiratory exercises performed before and after your operation can help to reduce the risk of lung problems by opening up your airways and moving phlegm. Respiratory exercises, coughing and walking after surgery can prevent post-operative chest infections and reduce your post-operative stay in hospital.
Practising respiratory exercises before your operation will make it easier to perform them afterwards. Here is our six-step guide to breathing exercises:
- sit upright in a supported chair
- breathe in and out normally
- take a slow deep breath in so that your ribs expand sideways and your lungs fill up with air and then exhale
- take a slow deep breath in and expand your lungs, hold that breath for three seconds and then slowly exhale
- repeat three times
- if you feel dizzy or tired return to breathing in and out normally.
Practise these respiratory exercises every two hours daily before your operation. After your operation you should practice them every one to two hours.
Eating well
Eating well before your operation will be crucial to your physical preparation and recovery from surgery. Cancer and cancer-related treatments are commonly associated with nutritional problems making it difficult for you to eat your usual foods. Consuming adequate nutrition in the form of energy and protein in the run up to your surgery will be important to:
- support your immune system and minimise the risk of infections
- give you the strength needed to ensure you are fit for surgery
Seeing a specialist dietitian can help you improve your nutritional status and quality of life. The dietitian will:
- assess your nutritional status by measuring your height, weight and grip strength
- review your blood test, diet, lifestyle, prognosis and treatment
- give you nutritional support and advice which may include changing the texture or types of food you eat, adding some high-calorie/protein supplements, advising on individualised weight loss strategies if you are very obese, or asking your GP to prescribe you with vitamins or minerals if your blood test shows any deficiencies
- monitor your progress and changing needs and adjust the advice given regarding your diet accordingly
Psychological wellbeing
Research shows that providing good quality personalised information to patients and their carers and relatives leads to better outcomes, reduced anxiety and improved patient experience. Our programme aims to give you information and support during all stages of your treatment. Your clinical nurse specialist (CNS) will meet with you at key intervals. This is an opportunity for you to discuss any concerns or uncertainties you may have. They will support you with decision-making, provide advice on side effects and symptom management, and provide emotional and basic psychological support throughout your treatment and recovery.
Your CNS will meet with you at key intervals to discuss your progress. They will explain your forthcoming treatments and give you information specific to your needs. They will support you with decision-making, provide advice on side effects and symptom management, and provide emotional and basic psychological support throughout your treatment and recovery.
Research also indicates that almost half of people with cancer find the emotional aspects of their illness the most difficult to cope with. It can also impact a patient’s relatives and/or carers. It’s very important for us to consider how you are thinking, feeling and coping with your diagnosis and your treatment at all times. Everyone in the team will be open to discussing these aspects with you at any time. We know that people often get a lot of relief and reassurance from speaking openly and feeling understood by their healthcare professionals.
The focus is on improving your self-confidence throughout the programme. This is done through well-established methods such as establishing short and long-term goals, providing feedback and connecting you with patients for peer support.
You’ll also be given some simple questionnaires to complete at the beginning of the programme and at other key points along the way. These will give us more information on your ability to cope, difficulties you may experience and your needs. The information you give us will not affect your treatment options in any way and will be kept fully confidential to the team of health professionals directly involved with your care. Your CNS will look at the results and discuss with you whether further support may be helpful. This could include:
- additional time with your CNS to talk through any concerns
- appointments with the clinical psychologists who are part of the hospital team and specialise in providing emotional and psycho-social support
- visiting one of our drop-in Macmillan information centres which are based at Charing Cross and Hammersmith hospitals
- visiting Maggie’s Centre at Charing Cross Hospital or The Lynda Jackson Centre at Mount Vernon Cancer Centre
If you have any ideas about what you’d find helpful or if you have any difficulties you’d like to address, please talk to us about it.
Your medication
Please bring a list of medications you are taking when you come to your outpatient appointment. Sometimes we may need to change or stop your medication at the time of surgery because they may lead to problems after surgery.
If you are in doubt about what medications to take and when to take them, please ask a member of your healthcare team.
Smoking and alcohol
Before your surgery it is especially important to stop smoking and reduce your alcohol intake.
Smoking
In addition to the general health risks associated with smoking, research has shown that smokers are more likely to suffer complications during and following surgery.
There is evidence to suggest the following benefits if you stop smoking before surgery:
- reduced risk of heart and lung post-operative complications
- decreased wound-healing time
- reduced length of stay
Alcohol
If you drink a lot of alcohol we recommend that you reduce the amount that you drink prior to your surgery. Alcohol can reduce the function of your heart and it also causes mild dehydration. However, reducing high alcohol intake suddenly when you come into hospital can also cause serious health problems, so it is better to cut down well in advance.
Enhanced recovery
Enhanced recovery is a post-operative care process which aims to ensure you are discharged as early and as safely as possible with the best possible outcome. The enhanced recovery team consists of surgeons, nurses, anaesthetists, dietitians and physiotherapists.
As part of the enhanced recovery process we will ensure that:
- you are in minimal pain
- you start eating well as soon as possible
- you walk as early as possible after surgery to expedite your recovery
- we minimise the use of tubes and drains
- you are able to ask questions about your recovery throughout.
Your healthcare team will inform you before surgery about your role and recovery in the post-operative period. This will help you understand what to expect and when to expect it.
Early activity is an important part of your recovery and will include:
- respiratory breathing exercises (see information above)
- coughing
- sitting out of bed
- walking as soon as possible after your operation and at least twice daily
Our outcomes so far
Approximately 100 patients have gone through the PREPARE for Surgery programme to date. Over the past three years since the programme was introduced, the rate of post-operative pneumonia has fallen from 60 per cent at the start of 2015 to 18 per cent by the middle of 2018, with a fall in the median length of stay from 14 days to 8 days over the same time period.
These improvements are likely to be multifactorial, with the PREPARE programme providing a proactive approach to physiological optimisation, physical conditioning, psychological wellbeing and patient engagement.
Our awards
- British Medical Journal Surgical Team of the Year 2017
- NIHR CLAHRC Brian Turley Award for Patient Involvement 2017
- British Medical Journal Patient Participation Award, 2017
- Venetia Wynter-Blyth: Royal College of Nursing Nurse of the Year 2016
- Royal College of Nursing Innovation of the Year award 2016
Imperial Health Charity
PREPARE for Surgery would not have been possible without the support of Imperial Health Charity, which has awarded a total of £162,000 to support the project over several years. The funding has been used to cover the initial pilot project and the programme’s continued development throughout its second phase.
Imperial Health Charity helps our hospitals do more through grants, arts, volunteering and fundraising. To find out more about the charity’s work and how you can get involved, visit their website.
About this page
- Last updated
