MRI tool that can diagnose difficult cases of ovarian cancer to be tested at the Trust
Imperial College Healthcare NHS Trust is going to be part of a major trial that will evaluate a new MRI tool for diagnosing ovarian cancer.
The new tool can identify cases of ovarian cancer which are difficult to diagnose using standard methods and has already produced encouraging results in a clinical study across 15 centres in Europe, including Hammersmith Hospital.
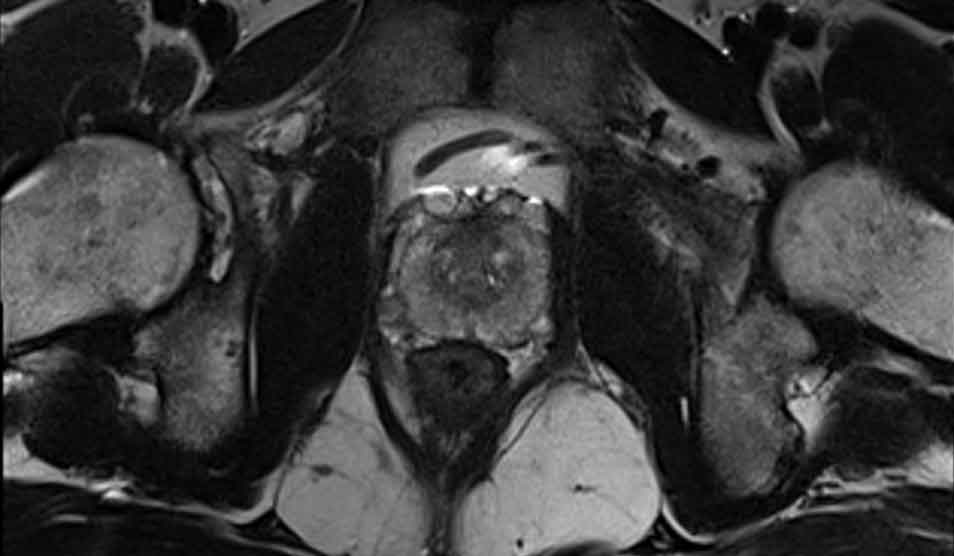
In the new study, researchers at the APHP-Sorbonne Université, with Professor Andrea Rockall at Imperial College London looked at the effectiveness of a tool called Ovarian-Adnexal Reporting Data System Magnetic Resonance Imaging (O-RADS MRI) in identifying the risk of cancer in ovarian cysts that could not be categorised by ultrasound in 1340 women.
Each patient underwent a routine pelvic MRI examination which looked for particular features in cysts that could not be identified during an ultrasound examination such as changes to tissue structure. A team of radiologists also analysed patients’ medical records and ultrasound scans to compare the tool.
The MRI tool was found to be able to distinguish between malignant (cancerous) and benign (non-cancerous) ovarian cysts with 90 per cent accuracy, in cases that cannot be distinguished on ultrasound.
The impact of the new MRI tool on the management and outcomes of women with ovarian cancer will now be evaluated in clinical practice at 18 hospitals in the UK, including at Imperial College Healthcare.
Currently, to investigate potential cases of ovarian cancer doctors use ultrasound scanning and blood tests. However, in a quarter of cases these methods cannot identify with confidence whether a patient’s cyst is benign or malignant. This leads to surgical investigations, which are invasive and carry risks, such as potential loss of fertility. In most cases women are then diagnosed as having benign cysts.
The team believes that the new tool can be used as a triage test to decide whether patients need further follow up or treatment. They also believe that the findings from the study, published in the JAMA Network Open, could help stratify patients who are high risk so they can be given treatment at a much earlier stage.
Senior author of the study, Professor Andrea Rockall, who is also a consultant radiologist at Imperial College Healthcare NHS Trust, said: “Ovarian cancer is referred to as a ‘silent killer’ as cases are often diagnosed at an advanced stage of the disease. When it is diagnosed earlier the chance of survival is much improved.
“There is a real unmet clinical need to find less invasive ways to identify women at risk of ovarian cancer. Our tool has the potential to help triage patients who are low risk so they can have less invasive treatment options, as well as identifying high risk patients so they can receive treatment at an earlier stage and have a better chance of long-term survival.”
Ovarian cancer is the sixth most common cancer in women and usually affects women after the menopause or those with a family history of the disease. There are 6,000 new cases of ovarian cancer a year in the UK but the long-term survival rate is just 35-40 per cent as the disease is often diagnosed at a late stage once symptoms such as bloating are noticeable. Early detection of the disease could improve survival rates.