Easing delirium in intensive care
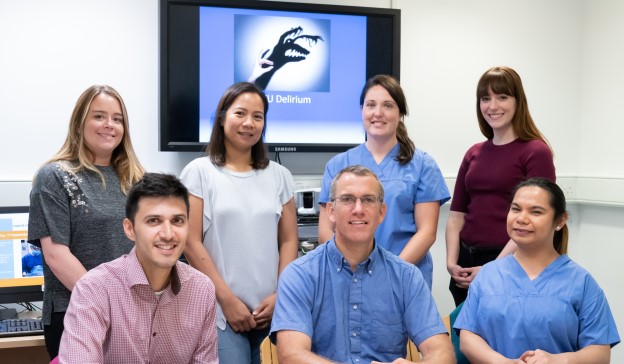
In 2018 consultant Chris Lambert and nurses Abigail Goodwin and Deirdre Moran started a delirium quality improvement (QI) project to improve delirium care in the Trust’s intensive care units (ITU). Here Abigail shares why this project is so important, and the learnings that have come out of it.
Typically described as a fluctuating disturbance of the mind, delirium can affect all patients at any age, but research suggests it affects patients staying in an ITU at a disproportionate rate, with over 80 per cent experiencing it at some point.
Despite being prevalent, it can often be difficult to identify, leading to increased length of stay, poor prognosis and poor patient outcomes. It has also been proven to increase morbidity and mortality.
My awareness of delirium first came about in 2017 when I did a project to improve patient flow in the ITU, before the unit expanded, and I noticed we weren’t treating delirium or training staff to recognise it. Following that I did an external intensive care course with the end project focusing on delirium, yet nothing progressed for a while. The turning point came when Chris joined the ITU at St Mary’s Hospital, and we established our shared interest in delirium.
In October 2018 Chris and I teamed up and, along with Deirdre, started organising a multidisciplinary team of staff who were interested in taking a delirium project forward. Split into multiple stages, the project aims to raise awareness of delirium across the Trust, improve diagnosis and treatment, and reduce incidence.
Stage one
The first part of the project looked at embedding the daily use of the globally recognised confusion assessment method for the ICU (CAM-ICU), to assess whether patients have delirium. The CAM-ICU uses a flowchart-like process to determine whether patients are negative – in which they do not have delirium, or positive – in which they likely do have delirium.
We conducted bedside teaching on the CAM-ICU to show nurses how to test for delirium, and then we showed them how to add the results to our online documentation system so that all staff members who needed the information could access it.
Using DREAMS to help patients
We’re currently in the middle of stage two, which involves looking at different interventions to limit the prevalence of delirium. Out of this has come the development of the ‘DREAMS rescue package’.
DREAMS: Drugs; Reorientate; Environment; Analgesia; Mobilise; Sedation and safety
This package contains a checklist to be completed by staff the first time a patient scores CAM-ICU positive. It prompts staff to check a number of factors: whether a patient uses a hearing aid, is thirsty, whether they smoke or take drugs, and so on. We once had a delirious patient who wasn’t interacting well, and all she needed was her glasses from home to help her settle.
Sometimes it’s the simple things that make a huge difference. The ITU environment is known for provoking delirium as there’s lots of noise and sometimes constant light, so we do what we can to improve that. We also use the DREAMS package to keep family involved, often asking them to bring in personal items such as pyjamas or a duvet.
Spreading the word
We’ve tried to be really positive about delirium and how we score it in order to get staff on board, and I particularly wanted to focus on hands-on teaching, so as part of this I had a staff member act as a patient and I set up a room like an ITU unit. I had loud alarms sounding, put mittens on the test-patient and blurred their vision, then I started prodding them without prior warning or explanation. It really shocked the rest of the team and helped them understand how this environment could exacerbate delirium.
Deirdre and I also packed a tea trolley we take around the unit full of teaching materials to quickly train staff and empower them to carry out CAM-ICUs and review the DREAMS checklist. We focused on positively empowering staff, and also feeding back how well everyone was doing.
Abigail Goodwin"Delirium can be very personal, and present differently from patient to patient. Classic symptoms to look out for, however, include: confusion; restlessness; rapid behaviour changes; withdrawal from interaction; lack of energy; and hallucinations"
Because delirium can present patients as confused and non-cooperative, staff can worry it will be difficult to put the training into practice, but it’s actually really simple. The DREAMS package provides clear, achievable ways to ease delirium, and it gives staff the confidence to treat it.
Delirium can also be a worrying concept for families, who often don’t understand the condition and worry it will last forever. Previously our nurses were not appropriately trained to explain how delirium works, and families and patients relayed that they felt there was a stigma attached so they didn’t ask questions about it. Our training has given staff the confidence to discuss it, and opened up the conversation for patients and their families.
Whilst Deirdre, Chris and I are based at St Mary’s Hospital, this project has been rolled out across all three of the Trust’s ITU units. Leading the charge at Charing Cross Hospital is consultant David Antcliffe, while educator Charlotte Styles leads training at Hammersmith Hospital. The outreach team also follows up with CAM-ICU positive patients who have gone to other wards.
Mapping success
Since we officially launched our project in March 2019 we’ve noticed better treatment of delirium on the unit, such as moving bed positions and utilising music therapy, and it’s clear that staff are putting their training into practice. We’ve also seen a massive improvement on our CAM-ICU scoring, which has now become routine.
A case that always sticks out in my mind is of a patient who presented positive delirious, and was clearly distressed. I decided to give her basic treatment to try and reorientate her, which simply involved taking the mittens she was wearing off, and minimising the wires attached to her. I also reassured her by reminding her where she was, and I helped to brush her hair. By the end of the day she was sat out of bed looking out of the window, and for me that was a huge achievement. For my colleagues to come round and see that she was fine, without the need for medication and simply by looking after her basic needs, was also a great teaching moment.
Once stabilised and out of delirium, patients themselves can often remember clearly how they felt during their ordeal, and we’re working to audit how their interventions are received by patients. Spoken feedback from patients has been positive, but we are in the midst of establishing a more formal way of getting this information and utilising it.
We’ve made good progress but there’s still a lot of work to be done. Through training and various interventions we hope to raise awareness of delirium across the Trust, and we want to encourage all staff to get involved in our project and learn more about how they can make a difference.
Everyone has a part to play in helping patients feel more comfortable and settled in our hospitals.
If you would like to find out more about the work intensive care are doing to tackle delirium, email abigail.goodwin1@nhs.net
Find out more about opportunities for nurses at our hospitals.
Share this blog on social media to join the conversation.


